Reuse
Currently, healthcare workers facing shortages in PPE, are being told to reuse existing items, often without sanitizing them appropriately. This section brings together the best available research to suggest how to make the best of this bad situation, so that PPE can be more safely reused.
Disinfecting N95 Masks
Considered the gold standard for protecting medical workers, N95 respirators or masks are able to block 95% of microscopic germs and particles that pass through its filter. These include both liquid droplets that contain germs like the SARS-CoV- 2 virus, as well much smaller suspended particles (~100 nm) of the virus itself.
At the heart of the N95 and surgical masks are polypropylene electret filters, which are polymer fibers that have charges imparted to them. These filters are able to remove microscopic particles through static attraction1 to the fiber, dramatically reducing the exposure of the virus to the wearer. Although multiple studies2 show that surgical masks prevent infection as well as N95 respirators do for similarly sized influenza viruses, the N95s have a better fit and capture more particles.
The WHO and CDC, along with mask manufacturers, do not encourage the reuse of N95 and surgical masks. Modifying a respirator invalidates its NIOSH certification, and OSHA requires that only NIOSH-certified respirators may be used in workplaces. However, with the global shortage of N95 masks, the CDC has introduced guidelines3 as a last resort for the limited reuse and extended use of N95 respirators.
To facilitate N95 mask reuse, the US FDA4 has begun fast-tracking decontamination methods for use by medical workers. Note: Masks should not be reused if soiled, torn, or used by a chronic patient. They should also be discarded if it no longer fits or cannot be breathed through efficiently.5
We have compiled below the latest information on decontaminating the N95 masks, with a focus on the N95 mask electret filter element. Use the content provided below solely at your own risk, as the efficacy and safety of sanitization has not been fully characterized across various N95 models. Consult the manufacturer to see which sanitization techniques are appropriate for your mask.
Process Suggestions across All Sanitization Methods
Masks should not be reused if soiled, torn, or used by a chronic patient.
Steps to follow:
1. Before sanitizing, you need to determine whether the other components of the respirator such as any plastic, metal nose piece, head and ear straps should be removed for a given procedure, and remove them before cleansing. For example, some masks also have paper-like outer or inner shells to hold the N95 filter, that may require a different technique.6 (See Appendix A for materials and their relative sensitivity to heat and other cleaning methods).
2. Before touching your N95 mask, you should wash your hands with soap and water or an alcohol based sanitizer; Don clean gloves; Avoid touching the inside of the N95 mask.
3. After sanitizing the mask and before donning the mask, you should wash your hands again.
4. Masks should always be returned to the original user after sterilization.
5. You need to then visually check to make sure the components have not degraded, and fit-test your N957 mask after sanitizing to make sure it is still sealed and conformed to your face, and make appropriate adjustments to ensure it is sealed properly.
6. If the components have degraded, replace them.
7. If the seal and fit do not function, then discard the mask.
Sanitization Methods That Work At Home
(Accepted by Experts)
~ 5 times
Oven/Blower
Cook mask at 70°C for 5+ min.
TIP: Be sure to suspend the masks in the oven without contacting or putting the masks too close to a metal surface using a wood or a plastic clip on its edge of non-breathing zone. Do not use metal grills. Put on a wood grill at least 6” away from a metal surface.
Rice Cooker
Cook for 3 min. Do not add water.
NOTE: This works for this mask model but not for this one because the latter has a plastic part in the interior that warps. ALSO, be sure to detach any metal nose pieces before performing, and then reattach and check fit before reuse.
Laboratory research has shown that the COVID19 (SARS-CoV-2) virus is rendered inactive by heat at 70° C (158° F) for five minutes.10 and masks at a slightly higher temperature 75° C (167° F) and time (30 min) do not deform and ear straps retain function11. (Appendix B)
In a recent press conference, the Taiwan FDA and Central Epidemic Control Center, endorsed using rice cookers (149~164°C (300~327°F), without adding water) for 3 minutes to disinfect the N95 masks, The Taiwan FDA states this method works for 5 cycles.12
~ 5 times
Microwave
Use a 1250-W (2450 MHz) commercially available microwave oven with a rotating glass plate to irradiate a single respirator per treatment for 2 min. Place the mask above a plastic box filled with 50 ml of room temperature tap water. The top of the box should be perforated with holes to evenly distribute steam over the entire surface. Place the respirator on top of the box with the convex end facing the steam.13
Stovetop
To do this, bring water to boiling with a wooden (not metal) dim sum tray insert so that it is above, but not immersed in water. Put the mask in the dim sum tray again with the convex side facing the steam for 10 minutes.
Convection Oven
In this video, a pulmonologist describes a method to sterilize both surgical and N95 masks with wet heat in a kitchen oven (convective) at 70°C for 30 minutes. The masks are placed over a wooden bowl to prevent melting and a separate bowl of water is placed in the oven to provide humidity.
Autoclave
NIOSH indicates that a minimum of 121°C (250°F) at 10 minutes is required but our bystander observation is that the temperature may be overkill.14
There is a consensus among experts that the SARS-CoV-2 virus can be deactivated at temperature between 65 °C and 80 °C (149 °F to 176 °F) at a relative humidity of 50% to 85% for a duration of 30 minutes.15 This is consistent with known observations of the related human coronavirus, which becomes less infectious at high humidities (80%).16
What is the ideal way to disinfect the N95 mask, to retain its function? In preliminary findings17, Stanford scientists found that application of steam (100 °C, 257 °F) to the polypropylene electret material over boiling water for 10 minutes can be an effective sterilization technique. They found that “filtration efficiency can be maintained (>95%) within 3 cycles, but the efficiency will degrade to ~85% after 5 cycles”.
Until soiled, torn, or used by a chronic patient or until breathing becomes difficult.
- Number four respirators (1, 2, 3, 4).
- Place each in a paper bag.
- Use #1 on day 1. At the end of day #1, put it in a new, clean paper bag labeled #1 with date used.
- Then, use #2 on day 2 with date used.
- Repeat on subsequent days with #3, #4, #5. Always use clean, new paper bags.
- On the 6th day, you can reuse the #1 mask, and continue the cycle.
Research indicates that the SARS-CoV-2 virus survives for up to 3 days on a plastic surface. As N95 masks are made of plastic polymer components, experts and organizations, including the CDC18 are suggesting they can be reused by placing used masks in a dry, breathable environment like a paper bag.
Sanitization Methods That Work In Industrial Settings
(Accepted by Experts)
419 to 20 times
Use an approved VHP system to expose the masks to aerosolized hydrogen peroxide. (Specialized equipment and personnel required to ensure safe implementation.)
NOTE: VHP can cause serious health effects. It is extremely irritating and corrosive, especially to mucous membranes such as those of the eyes, nose, throat, and lungs.20 If it escapes, it can be very dangerous since it is not easily detected, as it is colorless and odorless.
Researchers at Duke 21, have confirmed that vaporized hydrogen peroxide can decontaminate the masks so they can be reused. More recently, researchers at Virgina Tech22 have also shown that 3M’s N95 masks can be treated 10 times with 59% hydrogen peroxide vapor with little loss in filter efficiency. VHP is effective since vapor permeates the layers of the masks to kill germs, including viruses, without degrading the mask material.
In an effort to accelerate solutions to meet the shortage in protective N95 gear, the FDA at the end of March 2020 approved Battelle’s VHP system, which can clean up to 80,000 N95 masks per day. This enables the masks to be used up to 20 times. California has annouced plans23 in April to procure this system to reuse masks. Other VHP systems:
- In hospitals, Sterrad’s low temperature 100NX sterilizer system,24 which uses VHP, can process up to 480 masks a day. The company states their system can triple the lifespan of N95 masks.
- Tekdry,25 a startup, has a vacuum/hydrogen peroxide based system used to clean medical equipment and commercial electronics that has also been submitted for FDA approval to sterilize the masks.
Promising Technologies – Not Yet Fully Characterized
Ozone is a well-known decontaminant26, is a viricide, and can penetrate materials. It is a lung irritant so should only be used in a closed containment box or where humans are not present.
The filtration element of most N95 masks (blown polypropylene) is compatible with ozone27 but further research is needed to determine the amount of time needed for decontamination and the the number of use cycles for not only the filtration element for the other mask components.
UV-C is recommended for N95 mask decontamination and has a reuse limit of 10-20 times at a dosage of 1-1.25 joules/cm2.
The cautionary note is that UV-C deactivates viruses on the surfaces of the mask but may not reach the inner layers of all N95 models and may miss areas that are shaded from UV-C.28
While microwave irradiation is known to kill germs, data on SARS-CoV-2 is still lacking. Scientists have microwaved human parainfluenza29, an RNA virus similar to the COVID-19 virus in a petri dish for three minutes at 600 W. This experiment was enough to dactivate polio and parainfluenza viruses.30
Smart Air Filters31 scientists demonstrated that N95 filter function remained after microwave decontamination of N95 masks for three minutes. Prior to decontamination, any appendages to the filter, including the nose bar and metal clips, need to be disassembled (which is not recommended), but users can reassemble. Furthermore, the risk of melting or catching fire from microwave is real.
Where the microwave method could be effective at sterilising the mask material, it is most applicable for DIY masks that do not contain metal parts.
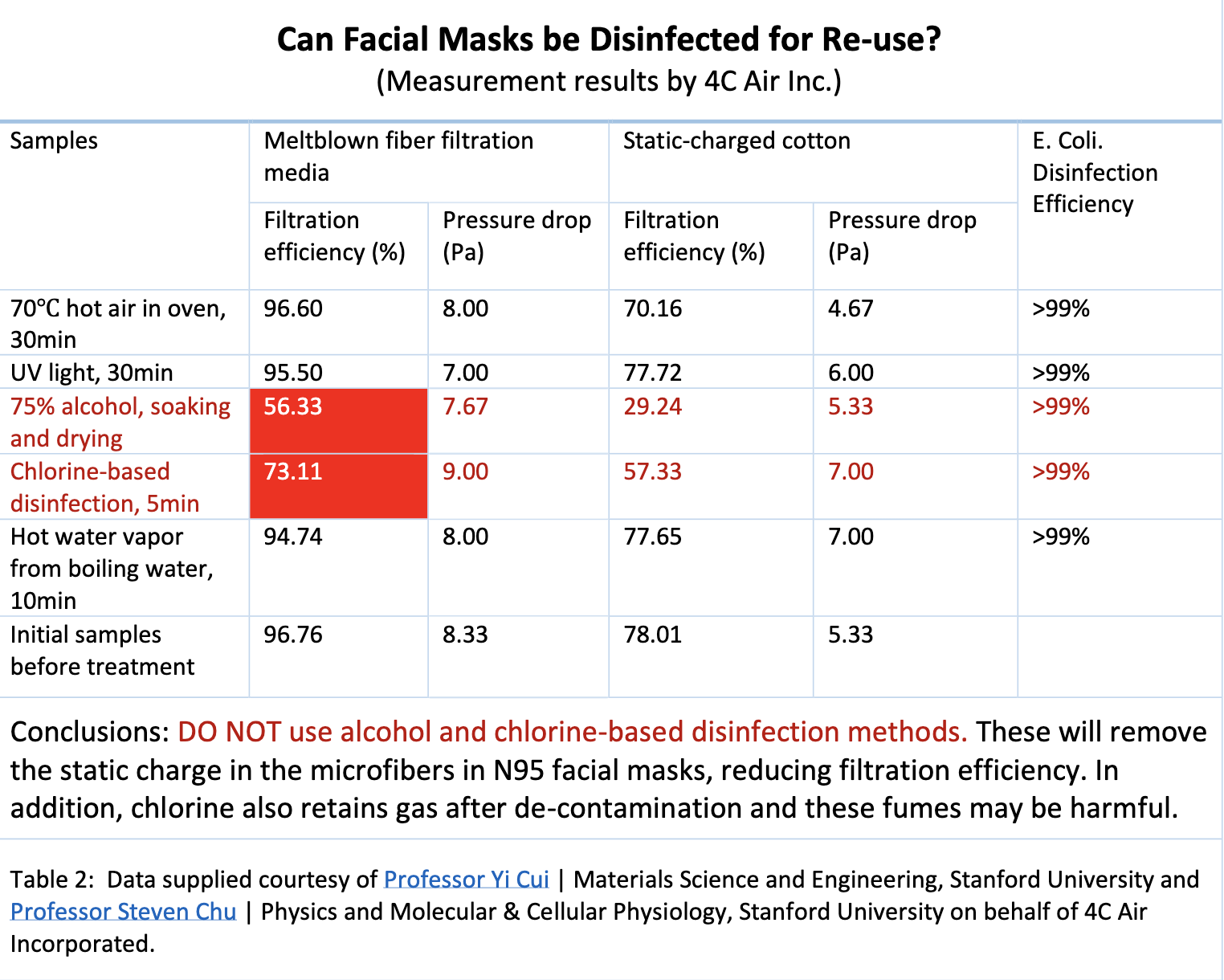
Not Recommended for N95 Masks
You may have seen some of these techniques online, but they are tested and do not work because they either damage the filtration or water repellency that are essential for the N95 mask’s functioning. They are not recommended.
Research has shown that the charge loss on the media is unnoticeable in boiling water for three minutes but stirring the mask is not recommended as it causes physical damage to the mask itself.32
Stirring is unavoidable in boiling, and stirring changes the physical composition of the mask.
Not recommended.
Alcohol is a common disinfectant but alcohol is not recommended for masks, because the mask is waterproof to block air droplets. Spraying alcohol dissolves the waterproof barrier33 as dramatically illustrated,34 and “removes the electrostatic charge from the filtration media and substantially degrades its filtration capacity.” 35
Alcohol also melted down fiber media for 4c Air filter.
Not recommended.
Chlorine does not work for one-time use face masks.
Not recommended.
Laundering will damage fit / shape of most masks.36
Not recommended.
Too difficult to control temperature, so not recommended for mask cleanup.
Appendices
Appendix A: N95 Mask Materials
Most N95 masks are made from a combination of polyethylene, polypropylene, synthetic rubber, and polyester materials. The key common component is a melt-blown polymer filtration layer – usually polypropylene — that has electrets that are permanently charged and can capture sub-micron particles. 37 Below 0.3 microns, the smaller the particle, the more likely it will be captured.
A table of common mask materials and their relative sensitivity to heat and cleaning methods is presented here. We recommend that you consult with the manufacturer about your mask model, the materials and construction before embarking on resanitizing the mask and its components.
Appendix B: Resources from studies
1. Stanford
2. Q&A with University of Tennessee Prof, Peter Tsai, inventor of the N95 Mask technology, on cleaning masks38:
Can the masks be sterilized by heat treatment?
Yes, it is reported (if it is true) that COVID-19 cannot survive at 65C for 30 minutes. Therefore, it is safe to sterilize the masks in hot air at 70C for 30 minutes and this process can be repeated multiple times to reuse the masks without a noticeable loss of efficiency. But be sure to suspend the masks in the hot air in the oven without contacting or putting the masks too close to a metal surface. The respirator can be hung in the oven using a wood or a plastic clip on its edge of non-breathing zone or put on a wood grill at least 6” away from a metal surface. Similarly, hold the edge of non-breathing zone when doffing the mask. Don’t touch the inside part of the mask because your hands might be contaminated at this time if the mask was. Wash your hands thoroughly using soap with water for at least 20 seconds according to CDC after donning the masks.
Can the masks be sterilized using alcohol?
No, face masks cannot be sterilized using alcohol because the charges will be erased by either alcohol liquid or its vapor as described in a previous section.
Can the masks be sterilized using radiation or UV?
It depends on the intensity and the exposure time. Radioactive such as gamma rays or UV light are commonly used for the sterilization of material but they have potential to decompose the PP material by the attacking of the lone pair electrons pairs in its CH3 side group on its backbone of the molecular chains leading to the dissipation of the charges. However, the degree of PP decomposition depends on the radiation and UV intensity as well as the exposure time. For example, the PP will be totally degraded and become brittle under sunshine in summer for three months. Someone needs to do the experiment to expose the masks to the UV or the radioactive intensity for the time that can kill COVID-19 and then measure the mask filtration efficiency to know.
Can the masks be reused after hanging dry?
According to a study published in New England Journal of Medicine (NEJM), The COVD-19 can survive in the air for three hours, four hours on a copper surface, 24 hours on a cardboard, two-three days on a stainless or a plastic surface. It is reported from CDC that the possibility of infection from a package being shipped for a few days from China is very slim, which is a similar result as in the NEJM. PP is a hydrophobic plastic material with zero moisture content. The virus needs a host – a cell – to survive. A respirator can get dry in less than two-three days in a dry air environment. Based on the above reports, three-four respirators can be numbered, let them get dry, and reuse in the numbered sequence.
Can the masks be sterilized using steam?
Yes, our investigation showed that the charge loss on the electret is unnoticeable by sterilization using 125oC steam for three minutes.
Can the respirator be sterilized by boiling water?
Yes, our investigation showed that the charge loss on the media is unnoticeable in boiling water for three minutes but stirring on the mask is not recommended to avoid its physical damage.
Can the respirator be in contact with water?
Yes, the charges of an electret, embed deep inside the fibers, are quasi-permanent. Different from the surface charges encountered in our daily life, they will not dissipate in the air or in contact with water. Our investigation showed that this electret had little charge decay after being immersed in water for three days. However, laundering should be avoided for its action will physically damage the masks.
In Q5, Q6 and Q7, to be sure that the inner or the outer veil of the mask is not made of paper-like tissues – paper pulp or nonwovens bond by water soluble binder, which will either dissolve in water resulting in loose fibers in the veil or the loss of its strength after exposing to water.
Disinfecting Gloves
Hospitals are facing a shortage in gloves. In particular, disposable rubber (latex) gloves are in short supply due to lockdown in Malaysia39 where most of the world’s gloves are made. Although there is little laboratory testing on this particular coronavirus, the American Chemical Society suggests COVID-19 to be one of the easier viruses40 to chemically deactivate. We posed the question to a chemist asking what that person would do if in that same situation to keep safe, with a focus on commonly available household chemicals.
Single-use gloves ARE weakened by physical use. Over time, microscopic holes develop weakening their tensile strength and efficacy. According to one study,41 after only 12 minutes of simulated clinical use increases defect rates of natural latex and vinyl glove 9 percent and 35 percent, respectively. There are real risks to reuse disposable gloves to both the wearer and the patients. This includes exposure to not only coronavirus, but also staph, norovirus, and MRSA.
The pointers below to resterilize single-use gloves are for emergency situations when supplies are limited. Neither glove manufacturers nor medical boards recommend the re-use of disposable gloves. In fact, researchers suggest that gloves be changed every 15 minutes42 to ensure safety.

Vinyl gloves

Latex gloves

Nitrile gloves
I. For medical professionals that need high tactile sensitivity: Vinyl, latex and nitrile are standard materials used for medical gloves: Vinyl is the cheapest, but weak and should not be reused. Latex is stronger but many people have latex allergies. It is the most appropriate in situations where medical professionals need to have a high level of tactile sensitivity. Nitrile is more chemically resistant but is the most expensive and may be more difficult to grasp instruments with. The quality and durability of the glove will also depend on the thickness, chemical finishes to the surface, and powders to control their stickability.
Suggested Process
1. Soap and water.43 To remove coronavirus, blood, bodily fluids, dirt, and other impurities on the gloves, wash the outsides in warm, soapy water while hands are in gloves. Then, turn the gloves inside out44 and soak them in warm soapy water for a few minutes. Then hang dry. The science of deactivating the coronavirus45 using soap is well established. Soap and water would probably get most of the way there. For more thorough sterilization, steps 2 and 3 are suggested, otherwise skip to step 4.
The above step #1 would remove most virus. If there is a very high standard, then move onto the other steps but be aware that each additional process reduces tensile strength, ie would affect the integrity of the gloves (may tear or have holes) if keep applying chemical or mechanical stress.
2. Chemical disinfection. To remove residual virus, apply Steramine or bleach similar anti-viral agent onto the outside of the glove using a cloth or wipe. Do not use alcohol as this will weaken the gloves. Apply for 10 minutes and let dry.
a. Steramine46 (milder than bleach) – Mix at least two and a half tablets of Steramine in one gallon of water for 500 ppm concentration (0.05%) solution of the QAC. Similarly, household Simple Green contains 0.15% of the active ingredient. A higher concentration of the QAC is acceptable.
b. Bleach (Sodium Hypochlorite) – Household Clorox Bleach is 7.4% concentration of Sodium Hypochlorite. Dilute to between 0.05% to 0.5% concentration through a dilution of between 1:150 to 1:15, respectively. NOTE: This should be carried out in a hood so bleach fumes do not hurt the user.
3. UV-C light. Expose dried gloves to UV-C lamp from within several inches for a period of a few seconds to cover entire outer surface of glove.47 This deactivates remaining RNA of viruses that may still be on the surface of the glove. NOTE: Should be carried out in a facility for disinfecting instruments. Hands and skin should not be directly exposed to the UV light.
4. Finish. Apply baking soda in your gloves. The powder will keep your hands and gloves smelling clean and fresh. Check for tears or holes. Store gloves in a dry, cool place. Sunlight and heat are not recommended as this can melt and damage the gloves.
II. For medical professionals that do not need high tactile sensitivity, re-usable gloves are preferred (eg. Rubbermaid reusable gloves): This conserves the high tactile sensitivity gloves for professionals that absolutely require them. In these applications, the gloves are not used for direct contact with patients or are not directly exposed to samples of the coronavirus. For these gloves, only steps 1 and 4 above need to be followed.